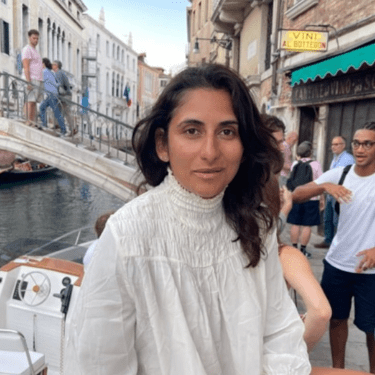
Healing from the Roots: Dr. Shreni N. Zinzuwadia’s Journey to Preventive, Integrative Medicine
Dr. Shreni N. Zinzuwadia has spent over two decades on the frontlines of emergency and trauma care, dedicated to treating patients in underserved communities. But her approach to medicine goes beyond simply managing symptoms. With a deep commitment to preventive and integrative care, Dr. Zinzuwadia empowers her patients to make meaningful lifestyle changes that support long-term wellness. Inspired by her own family’s struggles with metabolic syndrome, she has blended her expertise in acute care with holistic, evidence-based practices that target the root causes of chronic illness. As a physician of Puerto Rican and Indian descent, Dr. Zinzuwadia also understands the importance of culturally sensitive care and representation. Her vision? A future where health and prevention are accessible to everyone, breaking cycles of illness and building a healthier, more resilient world.
What inspired your shift toward an integrative and preventive approach in medicine?

As an emergency physician with two decades of experience, I am an expert in delivering trauma care and acute care. In the Emergency Department, I have seen countless cases of the end stages of all kinds of chronic illness-diabetes, hypertension, heart disease, stroke, cancer, and auto-immune disease. The patients I have taken care of in the Emergency Department come for help so late in their disease process that the conventional treatment I offer is most often an attempt to save their lives. But this is too little too late.
Driven by a desire to do more, I started my journey to becoming an expert in functional medicine, obesity medicine, and lifestyle medicine. I have learned that a more holistic approach—one that respects the body’s innate ability to heal—is essential.
How have the healthcare needs of underserved populations changed over your career?
For the past 23 years, I have been dedicated to caring for underserved populations, a commitment that began with my medical training in Newark, NJ. I completed my medical school and internal medicine internship there, where I first encountered the pressing health disparities affecting vulnerable communities. My emergency medicine residency in the Bronx deepened my understanding of the unique challenges these patients face, and I continued this work with two years of service in Brooklyn. For the past 14 years, I have returned to Newark, where I strive daily to provide compassionate, accessible care to those most in need. This journey has solidified my commitment to bridging healthcare gaps in underserved communities. .
Serving diverse populations for over 20 years in urban, suburban, and rural settings has shown me how many people face barriers to optimal health due to systemic disparities. I serve patients who face a high prevalence of metabolic syndrome and other preventable chronic diseases. Culturally sensitive, preventive approaches are needed in treating chronic illness. My journey has solidified my commitment to bridging healthcare gaps and empowering underserved communities to lead healthier lives.
How has your family’s experience with metabolic syndrome influenced your medical approach?
With our strong genetic predisposition to metabolic syndrome, I have seen many of my family members suffer—and some have even lost their lives—from complications related to metabolic syndrome. My grandmother died of complications of a massive stroke, which was a complication of her Diabetes, High blood pressure, and dyslipidemia. I have two maternal uncles who also died of complications of metabolic syndrome. One died of a silent massive heart attack. The other one died of a diabetic coma. This has given me a deeply personal understanding of the devastating effects this condition can have on individuals and families. Witnessing these losses firsthand has left an indelible mark on me, driving my commitment to exploring a more comprehensive approach to health and healing, one that addresses both the prevention and management of chronic conditions like metabolic syndrome.
What barriers to health have you observed in urban communities like Newark, the Bronx, and Brooklyn?
In urban communities like Newark, the Bronx, and Brooklyn, I’ve seen multiple barriers to health, including limited access to healthcare, financial constraints, and language barriers that make navigating the system challenging—especially for non-English speakers. Many residents face low health literacy, making it difficult to understand preventive measures or treatment options. Additionally, food deserts and the high cost of fresh, healthy foods lead to diets reliant on processed foods, contributing to obesity and chronic conditions like diabetes. Environmental stressors, such as pollution and crowded living spaces, further impact both physical and mental health, creating a complex web of challenges for these communities. These phenomena are not limited to the inner cities. They exist in rural critical access areas as well.
How does blending integrative and conventional medicine shape your patient care today?
My integrative medicine approach aligns perfectly with my vision of offering the needed holistic approach to bring people to health. I can support my patients in achieving true wellness, not merely the absence of disease, by bringing these principles to their lives.
How do you incorporate cultural awareness into your practice to improve patient outcomes?
A culturally sensitive approach to care, informed by my background as a Puerto Rican and Indian physician, allows me to bridge these gaps by offering accessible, integrative care to communities that need it most. My journey, coupled with my genetic predisposition, gives me a unique perspective that resonates with many of my patients, particularly those from minority communities who share similar health risks. My goal is to empower these individuals to make proactive lifestyle changes that could shift the course of their health, breaking the cycle of chronic illness for future generations.
What strategies do you use to encourage patients to prioritise long-term wellness over symptomatic relief?
I encourage patients to focus on long-term wellness over quick fixes. I educate them on the importance of addressing root causes, explaining how preventive measures can lead to lasting health improvements. I help them set personalized, achievable goals and track progress in key areas, allowing them to see the benefits of their efforts over time. By providing empathetic support and emphasizing how wellness enhances the quality of life, I guide patients to understand that prioritizing their health today means a healthier, more fulfilling tomorrow.
How can healthcare systems shift from reactive treatments to preventive care?
Healthcare systems can shift from reactive treatments to preventive care by implementing several key changes. First, they can invest in public health initiatives that promote education on healthy lifestyles, nutrition, and preventive screenings, making preventive care accessible and understandable. Systems should prioritize early intervention programs and regular screenings, especially in high-risk populations, to detect and address health issues before they become severe. Integrating holistic approaches—like lifestyle medicine, mental health support, and wellness coaching—into standard care helps patients focus on long-term health, not just symptom management. Additionally, healthcare policies and insurance models should incentivize preventive care, making it affordable and rewarding for patients and providers alike. Finally, training healthcare providers in preventive and integrative medicine can encourage a proactive mindset, ensuring that the focus remains on keeping patients healthy rather than solely treating illnesses.
What changes do you hope to see in healthcare, particularly in integrative medicine, over the next decade?
Over the next decade, I hope to see a fundamental shift in healthcare, particularly in the realm of integrative medicine. One key change I envision is a more holistic view of the human body—not as separate organ systems, but as an interconnected set of physiological systems that influence one another. This approach would mean treating patients as whole beings, acknowledging how factors like mental health, nutrition, lifestyle, and environment interact to impact overall wellness. By fostering this integrative perspective, we can move toward treatments that support the body’s natural healing processes, ultimately leading to more effective, sustainable health outcomes. I believe this shift will encourage a preventive, patient-centred approach, focusing on maintaining health and preventing disease, rather than merely responding to isolated symptoms or conditions.
What legacy do you hope to leave in the field of integrative and preventive medicine?
I have a vision of reshaping healthcare in the U.S. by blending integrative and conventional medicine. I believe in a future where wellness and prevention are central to patient care, and where individuals from all backgrounds have the support, they need to thrive. I bring these life-changing benefits to my patients and community. Through my work, I aim to honour my family’s legacy and empower others to live healthier lives.
APPLY TODAY
100 Top Global Women Entrepreneurs – Global Woman Magazine
Our Journey in 12 Months:
Our Journey in 12 Months – Global Woman Magazine
5 Things That Show Money is Not Evil:
5 Things to Show That Money Is Not Evil – Global Woman Magazine
Global Man Magazine Page:
Global Woman, Global Man: Socials:
Global Woman Magazine (@global_woman.magazine) • Instagram photos and videos